
Varicose veins most commonly affect the venous system in the legs. External manifestations (raised blue veins, swelling) are not just a cosmetic problem but a sign of a serious disease that gets worse over time.
What are varicose veins: disease definition
The word "varicose veins" comes from the Latin word varix - "swelling". This name fully reflects the pathological process: the walls of the veins become thinner and bulges (sac-like swellings) - nodes - form in some areas.
The first case of varicose veins was recorded in a document from 86 BC. BC: Roman general Gaius Marius complained of pain in his legs from "blue swollen veins".
The main reason for the development of varicose veins (varicose veins, varicose veins) is an increase in pressure in the superficial vascular system. This is facilitated by certain diseases, hormonal changes and a sedentary lifestyle.
At first, even under the influence of these factors, blood vessels still function normally, but gradually they become deformed, change their structure and are no longer able to adequately transport blood.
Varicose veins can develop in almost any part of the body, but most commonly appear in the lower limbs. So when it comes to varicose veins, by default they mean leg problems.
ICD-10 varicose vein code
The International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) includes several types of varicose veins.
I83 - varicose veins of the lower limbs:
- I83. 0 - varicose veins of the lower limbs with ulcers;
- I83. 1 - varicose veins of lower limbs with inflammation;
- I83. 2 - varicose veins of the lower limbs with ulcers and inflammation.
85 - esophageal varices:
- I85. 0 - esophageal varices with bleeding;
- I85. 9 - Non-bleeding esophageal varices.
I86 - varicose veins in other localities:
- I86. 0 - sublingual varicose veins;
- I86. 1 - scrotal varices (anatomical formation in men - where the testicles and their appendages are located);
- I86. 2 - pelvic varicose veins;
- I86. 3 - vulvar varicose veins (female external genitalia);
- I86. 4 - gastric varices.
O22. 0 - varicose veins of the lower limbs during pregnancy.
In our country, 30 million people suffer from various forms of varicose veins. A third of them have complications - trophic ulcers. An open defect in the skin or mucous membrane that occurs due to impaired blood circulation and tissue innervation.
Mechanism of development of varicose veins
The body's pathological reactions are the same for all types of varicose veins, regardless of the cause of the problem. Understanding the anatomy of blood vessels will help understand how and why the disease develops.
How blood moves in the body
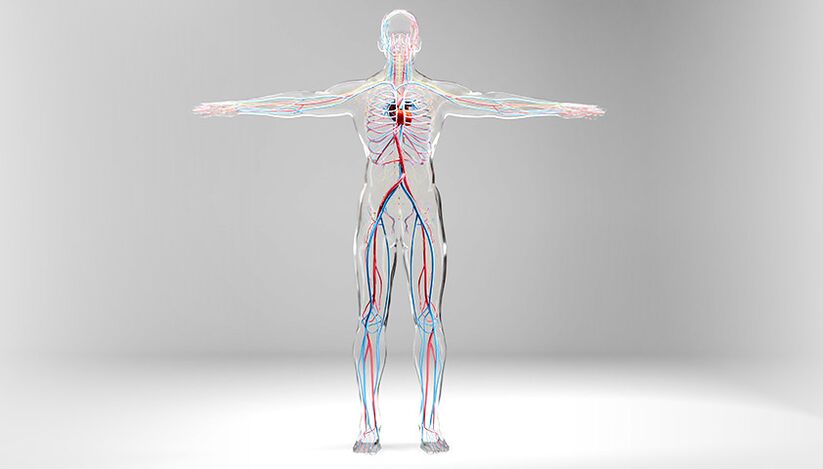
There are two types of vessels in the human body - veins and arteries. Blood flows through the arteries from the heart to all organs and tissues. This occurs under high pressure (70–120 mm Hg) and at high speeds.
Blood flows through the veins from organs and tissues, and it is carried back to the heart under low pressure (0–20 mm Hg).
Venous walls are less thick and elastic than arterial walls, and unlike arteries, do not contain such a developed muscle layer. Therefore, varicose veins can only occur in veins and not in arteries.
Human arterial and venous circulatory system. Veins are shown in blue, arteries in red.
Low pressure in the veins is necessary to transport blood from the periphery to the center. But at the same time, on the way to the heart, the bloodstream encounters an obstacle - the force of gravity. This force forces the blood back through the veins.
You can often hear that varicose veins are humanity's retribution for walking upright. After all, the longest distance blood has to travel in the body to overcome gravity is from the feet to the heart. The movement of blood through the veins is ensured by the contraction of the heart, the pumping force of the surrounding muscles and the negative pressure in the chest during inhalation.
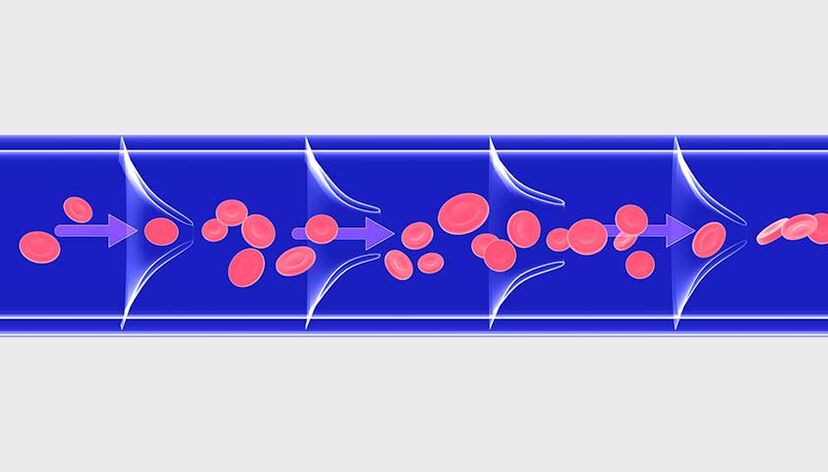
In healthy vessels, backflow of blood is prevented by valves on the inner walls of the veins. The valves act like one-way revolving doors - they open and allow blood to flow to the heart and immediately close if gravity tries to push the blood out.
Not only do the valves help the veins carry blood to the heart, but also the muscles that surround the vessels. By contracting and relaxing, muscles help blood move through the veins. This mechanism only works when a person moves. When standing or sitting for long periods of time, muscles are practically inactive.
The tips of the venous valves always point toward the blood flow - toward the heart
How failures happen and illnesses happen
An increase in pressure in the venous system disrupts the functioning of the valve apparatus and leads to a backflow of blood through the vessel. Because of this, as well as due to excess blood stagnation, weak valve apparatus (for example, in connective tissue diseases), the vein lumen dilates, the walls are deformed, become thinner and resemble local sacs. protrusions - nodes - are formed.
The process is similar to inflating a balloon: if you don't let the air escape, the balloon will inflate more and more.
On the left is normal blood flow; on the right - multidirectional blood flow due to impaired function of venous valves, vascular deformation

In the legs there are superficial and deep veins. 85–90% of the total blood volume passes through the deep zone, only 10–15% through the superficial zone. The walls of deep veins are denser and more adapted to increased blood volume. And the superficial veins in the legs are thinner and more susceptible to varicose veins.
In the pelvis and lower part of the esophagus there are large venous plexuses, which can also be transformed into varicose veins. In the small iliac veins, the mechanism of disease development is the same as in the lower limbs. But esophageal varices arise for another reason: due to portal hypertension - increased pressure in the portal venous system, which develops with cirrhosis, hepatitis, parasitic liver damageinfections, fatty liver, etc. v.
Causes of varicose veins
Several factors contribute to the development of varicose veins in the legs. The main ones areheart valve failureAndheredity. It is known that 1/4 of patients have a relative suffering from one of the types of varicose veins.
Overweight. The more pounds a person has, the greater the load on the venous system. Over time, the veins can no longer withstand such pressure: the brightness of the vessels increases, and the valves on their walls no longer close completely. As a result, blood stagnates and varicose veins develop.
Pregnant. Hormonal changes occur in the female body, body weight, intra-abdominal pressure and circulating blood volume increase - this leads to disruption of outflow, causing tension in the walls. veins and changes in the functioning of the valve apparatus.
After childbirth, the diameter of varicose veins decreases but does not always return to the original value. With subsequent pregnancies, the risk of varicose veins increases.
Year old. Varicose veins often affect people after the age of 50. The older a person gets, the more the venous valves wear out, at the same time the recovery process slows down and the mechanism of pathological expansion of the veins is activated - the development of varicose veins.
Venous refluxVenous refluxBlood returning to the veins due to obstruction of blood flow, from lat. refluo - "backflow. " found in 10–15% of students aged 12–13 years. The "rejuvenation" disease is caused by a sedentary lifestyle and being overweight.
Varicose veins of the lower extremities develop more quickly if additional risk factors are present.
Risk factors that contribute to the development of varicose veins in the legs:
- lack of physical activity - when moving, muscles stimulate blood flow through the veins, and without exercise, blood circulation in the veins can be difficult;
- smoking - chemicals contained in cigarette smoke damage the walls of blood vessels, as a result of which their lumens narrow, blood flow becomes difficult and stagnation occurs, which leads to varicose veins;
- Occupations that require standing or sitting for long periods of time - hairdressers, surgeons, chefs, waiters, drivers, office workers are at risk;
- menopause - in women 40–50 years old, the production of sex hormones (estrogen and progesterone) decreases, and the tone of the vein walls also decreases. This increases the likelihood of varicose veins.
Women have varicose veins 3-4 times more than men. This happens due to hormonal changes (menstrual cycle, pregnancy, menopause).
During pregnancy, varicose veins can affect different parts of the body: legs, thighs, vulva

Varicose veins can occur not only in the lower limbs, but also in other parts of the body.
The main cause of varicose veins in many different locations
Esophageal varices
Changes in the veins of the esophagus with irregular increases in their lumen, protrusion of the walls and development of tortuous nodules of the vessels. Often leads to a life-threatening complication - bleeding.
Reason:
- cirrhosis
- liver cancer
- Other diseases cause increased pressure in the portal venous system - it collects blood from the abdominal organs
Varicose veins of the scrotum (varicocele)Pathological dilation of the veins of the pampiniform plexus of the testicles. Presents with varicose veins in the scrotum and impaired blood flow
Reason:
- Congenital weakness of the testicular venous valves (usually the left valve)
- mechanical compression of the testicular vein (inguinal hernia)
Pelvic varicose veins
It is characterized by dilatation of the ovarian veins and intrapelvic venous plexuses of varying diameters. This condition is also known as pelvic congestion syndrome
Reason:
- polycystic ovary syndrome
- two or more pregnancies
- endocrine disorders
Varicose veins of the vulva
Pelvic varicose veins, which affect the blood vessels of the labia and perineum
Reason:
- The uterus compresses the retroperitoneal blood vessels during pregnancy
- significant physical activity
- Tumors of the uterus and ovaries
Varicose veins under the tongue (varicose veins under the tongue)
Asymptomatic lesions in the veins located under the tongue. Appears as slightly protruding blood vessels and changes in color from dark blue to purple
Reason:
- high blood pressure
- smoke
- age
Gastric varicose veins
Changes in gastric veins alone or in combination with esophageal varices
Reason:
- cirrhosis
- portal hypertension syndrome - increased pressure in the portal venous system in other gastrointestinal diseases (neoplastic tumors, thrombosis, abnormalities of venous development)
Symptoms of varicose veins
In rare cases, the disease appears only cosmetically - blue veins. Most patients with varicose veins in the legs report at least one or more unpleasant symptoms.
Symptoms of varicose veins of the lower limbs:
- fatigue, pain or heavy feeling in the legs - this is caused by blood stagnation and pressure on surrounding tissues;
- burning, tingling or pulsing in the legs - a reaction that slows blood flow and overflows the venous system of the lower limbs;
- muscle cramps at night - painful spasms that occur due to blood stagnation and accumulation of metabolic products in tissues;
- swelling of the feet and ankles - due to stagnation in the veins, the liquid part of the blood seeps into the subcutaneous tissue through the altered walls of the vessels;
- itchy skin around damaged veins - dilated and altered blood vessels do not provide normal blood circulation and nutrition to the skin, so the skin dries out and becomes rough.
The feeling of discomfort in the legs in patients with varicose veins increases in the evening, especially after long periods of sitting or standing.
The appearance of altered veins is not always proportional to the severity of symptoms. Therefore, veins that are difficult to see with the naked eye and are affected by varicose veins can cause serious discomfort, while veins that are prominent and thickened can cause little concern.

Varicose veins affect different veins: from small vessels of the skin to the great saphenous vein
Symptoms of other types of varicose veins largely depend on the underlying cause of the disease. Usually the patient does not complain about anything, and the doctor identifies the problem only during examination. This happens, for example, with sublingual varicose veins.
In some cases, as with esophageal or gastric varices, the pathology immediately manifests itself as a life-threatening complication - bleeding.
Classification of venous diseases
In clinical practice, doctors rely on the international classification of venous diseases - CEAP. This is an abbreviation formed by the first letters of the main parts of the classification:
- C - clinic (clinical change);
- E - cause (origin of the disease);
- A - anatomy (anatomical localization of varicose veins);
- P - pathogenesis (mechanism of venous blood flow disorders).
Complications of varicose veins in the legs
Usually, varicose veins themselves are not life-threatening. But sometimes the disease can cause complications.
Thrombotic phlebitis- inflammation of the vein wall, accompanied by the formation of thrombus (blood clot) blocking the vessel lumen. It presents with swelling and redness along the affected vein. The patient feels pain, the skin in the affected area becomes red and hot to the touch.

Thrombophlebitis is an inflammatory reaction of the skin and subcutaneous tissue along a thrombosed vein.
Venous trophic ulcers- open defects of the skin and soft tissues due to blood stagnation, edema and impaired cellular nutrition. Ulcers occur on the legs and ankles near the area of varicose veins. On the lower part of the leg, the swelling is more pronounced, meaning the tissues are compressed more than in other areas. Ulcers take a long time to heal and they often contain bacteria, which increases inflammation.
Nutritional ulcers heal very poorly due to impaired blood circulation and tissue nutrition

bleed- Occurs when veins rupture or dilate due to varicose veins. In the later stages of the disease, the skin over such veins is very thin and dry - a small wound is enough to compromise the integrity of the vessel and cause bleeding. Sometimes spontaneous vein rupture occurs in areas with varicose veins.
Diagnosis of varicose veins in the legs
A phlebologist deals with the diagnosis, treatment and prevention of venous diseases. The doctor makes a diagnosis based on the patient's complaints, examination and instrumental studies. If the symptoms of varicose veins are pronounced, tests are usually not indicated: just seeing a doctor is enough.
Your doctor may prescribe laboratory tests to prepare you for surgery or to rule out concurrent diseases that affect the condition of your blood vessels.
One of those diseases is diabetes. It may worsen varicose veins and increase the risk of complications (especially trophic ulcers).
To make an accurate diagnosis and determine treatment tactics, you will need a duplex ultrasound - the gold standard for diagnosing vascular conditions. This method allows you to evaluate the structure, function, strength of superficial and deep veins, the consistency of the valves, and also determine the direction of blood flow.
If secondary varicose veins are suspected (which can occur after deep vein thrombosis), the doctor will prescribe a venogram, CT scan or MRI.
Phlebography is an X-ray examination used to determine the condition of deep veins and valve function.
Computerized or magnetic resonance venography is used to visualize the venous system in three-dimensional projection and at very high spatial resolution.
Treatment of varicose veins in the legs
The goals of treating varicose veins are to reduce or eliminate symptoms, improve the appearance of the veins, and prevent complications.
Doctors choose treatment depending on which vessels are affected and how severe the patient's varicose veins are.
Non-invasive treatment method
Non-invasive treatments for varicose veins include compression therapy, drug treatments, and lifestyle changes.
Compression therapy involves wearing special socks, stockings, and tights. The choice of design, fabric type and level of compression depends on the symptoms. Your doctor will help you choose the right hosiery.
Compression vests on the lower legs compress more than on the upper legs - thereby pushing blood back to the heart and eliminating stagnation

Effects of compression therapy on varicose veins:
- manifestations of reduced symptoms - heaviness, leg fatigue, night cramps, burning sensation or pain;
- The severity of edema is reduced due to improved blood circulation;
- Healing of trophic ulcers is accelerated because elastic compression improves blood circulation and tissue nutrition.
Drug treatment - the doctor may prescribe Phlebotropic drugs (phleboprotectors, venotonics) Biologically active substances that increase venous tone and reduce the severity of venous-specific symptoms. (intravenous drugs).
The main groups of phlebotropic drugs used for varicose veins:
- Vasoprotective drugs: improve microcirculation, normalize increased capillary permeability, reduce blood viscosity and clotting ability;
- antithrombotic drugs: reduce the risk of dangerous blood clots (thrombosis) forming in blood vessels and promote the dissolution of existing clots;
- bioflavonoids: natural plant compounds that help improve venous tone and reduce venous congestion.
Lifestyle changes for varicose veins significantly slow down the progression of the disease and in combination with other recommendations of the attending physician will help stop the pathological process.
Important directions in changing the lifestyle of patients with varicose veins:
- moderate-intensity exercises: walking, swimming, water aerobics, leg exercises, yoga. Strengthening the muscles will help normalize blood circulation in the vessels, reduce venous stagnation and edema;
- weight control: thanks to the normalization of body weight, the load on blood vessels is reduced and the return of blood through the veins to the heart is facilitated;
- give up bad habits: nicotine and alcohol damage the inner walls of blood vessels and disrupt the regulation of vascular tone. Quitting smoking and drinking alcohol improves vein health and valve function.
Invasive methods of treating varicose veins
Invasive treatments include medical procedures that affect the integrity of the skin or mucous membranes. Sclerotherapy is a procedure that uses a special sclerosing solution (sclerosing agent). The solution is injected into the problematic vein through a thin needle, causing it to sclerotic - "stick together". Veins are shut off from the bloodstream and become invisible over time; Its function is taken over by neighboring veins. Sclerotherapy is performed without hospitalization - after the procedure, the patient can go home.
The sclerotherapy procedure takes from 5 to 30 minutes, depending on the number of varicose veins that need to be filled with sclerosant and their size.

Endovenous laser thermal ablation (EVLO). A catheter guided by laser light is inserted into the vessel through a small incision. The laser's thermal energy heats the vein, and it becomes obliterated—"sealed. "After a few months, the blood vessels are replaced by connective tissue and disappear. The procedure is performed on an outpatient basis.
Radiofrequency vein ablation (RFO) is the impact of high-frequency electric current on the inner surface of a blood vessel. Through a micropuncture, a catheter is inserted into the vein, which is connected to a device that generates radiofrequency pulses. Inside the vessel, radio waves are converted into heat energy, "sealing" the vein.
With EVLO, the vein is exposed to high temperatures for short periods of time; With RFO, the temperature is lower but the treatment time is longer. Both procedures are effective and safe.
Removal of NTNT, or non-thermal blistering methods:
- vein removal with cyanoacrylate glue;
- mechanical destruction, in which simultaneous mechanical and chemical impacts occur on the vessel.
NTNT removal is the most modern, least traumatic method to treat varicose veins with a short recovery time.
Phlebectomy is the removal of varicose saphenous veins. It can be performed as a stand-alone activity or in combination with other techniques. Varicose veins are removed under local anesthesia through small punctures.
Preventing varicose veins in the legs
You can prevent the development of varicose veins if you follow simple prevention rules in everyday life.
The combination of triggers – sitting cross-legged for long periods of time, wearing uncomfortable shoes – increases the risk of varicose veins in the legs.

Preventing varicose veins - what you need to know:
- moderate physical activity (walking, swimming, leg exercises) and rest with legs elevated improves the free movement of blood through the vessels and helps avoid stagnation in the veins;
- Proper nutrition and normalization of weight lead to strengthening of blood vessels;
- Wear loose clothing that does not restrict movement to help improve blood circulation;
- Cool bathing in the warm season helps tone veins;
- Comfortable shoes with a low heel (no more than 3 cm) help avoid inappropriate load on the foot and disruption of blood flow;
- A rational approach to visiting the sauna and steam bath allows you to maintain normal blood flow (long-term hot compress procedures greatly dilate the veins, as a result of which blood flow slows down).

























